Abstract
Background: We undertook a large multisite observational study (the ESCAPED Trial), collecting prospective data on experiences of care for adult patients with sickle cell disease (SCD) who were being treated in the acute setting for a painful vaso-occlusive crisis (VOC). Our aim is to compare patient centered outcomes following management of acute VOC events in the emergency department or in the infusion center. Acute care in the emergency department (ED) has historically been marked by long delays, lack of efficacy, and conflict. SCD patients report not having enough involvement in decisions about their own care and also that providers do not demonstrate respect, trust, and compassion. Little is known about patient's perception of safety in the acute setting and this issue was raised by our PCORI patient advisory council prior to the start of our study. Here, we examine patient's perception of safety in the acute care setting.
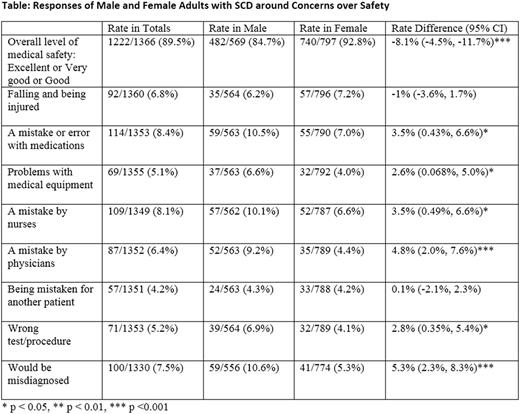
Methods: The ESCAPED Trial is an ongoing, prospective cohort study that is recruiting across four sites (Baltimore, Cleveland, Milwaukee, and Baton Rouge). 483 adults with SCD who live in proximity to one of the study sites have been recruited and are being followed for 18 months. Data from visits for all acute, uncomplicated VOCs are collected and participants are asked to complete a survey within 72 hours of their acute visits. Included in the survey are questions about perceptions of safety. We tested for associations between subject characteristics and perceptions of safety using a generalized linear mixed model including a random intercept to control potential clustering within subjects. The questions about safety included in the study were: Overall level of medical safety (defined as ''freedom from any medical error or mistake'') you felt during your acute stay with a 5 point Likert response varying from excellent to poor and During your acute visit, were you ever concerned that any of the following would occur?: 'Falling and being injured', 'A mistake or error with medications', 'Problems with medical equipment', 'A mistake by nurses', 'A mistake by physicians', 'Being mistaken for another patient', 'Wrong test/procedure' or 'Would be misdiagnosed' with yes/no responses.
Results: The average length of follow-up to date is 16.2 months with a range of (6-18) months. This analysis includes 324 subjects (324/483, 67%) who have had acute visits during the study period. These 324 subjects have had 2250 acute visits and this analysis includes 1366 survey responses from those visits. 60.5% of the sample are female, the average age of subjects is 33.8 years. The mean number of visits is 10.7 (sd 13.7) with a range of (1- 81). Participant responses can be found in the Table. In multivariate analysis, controlling for place of visit, male subjects were 63% (95%CI: 32% to 80%) more likely than women to report that the level of medical safety during their acute visit was only fair or poor. Male subjects were 3.64 (95%CI: 1.24, 10.63) times more likely to be concerned about problems with medical equipment, 2.87 (95% CI: 1.32 to 6.24) times more likely to be concerned that a physician would err, and 3.46 (95% CI: 1.41 to 8.50) times more likely to think that they would be misdiagnosed compared to female respondents. There were no sex differences in concerns over falls, being mistaken for the wrong patient, that nurses would err, that there would be a medication error or having the wrong test/procedure performed.
Conclusions: Acute care visits for adults with sickle cell disease are often described as dehumanizing experiences by patients. While there are a number of aspects of care including provider-patient communication that are relevant to these visits, we explore here how concerns over safety may add to the stress of these acute care visits. For most patients surveyed, concerns over safety were minimal. However, in almost 15% of visits, male patients with SCD reported a perception of a significant lack of medical safety. In 10% of visits by male subjects, there were concerns over medications errors, over errors by nurses, and over being misdiagnosed. Visits by males were significantly more likely to be associated with concerns over safety issues than visits by women. Further study is needed to better understand this novel observation and what underlies these concerns, what interventions can be developed to decrease these concerns, and importantly what impact these have on the overall care of our patients.
Lanzkron: HRSA: Research Funding; Bayer: Research Funding; Global Blood Therapeutics: Research Funding; Pfizer: Research Funding; PCORI: Research Funding; Prolong: Research Funding. Seufert: PCORI: Research Funding. Little: Hemex Health: Equity Ownership. Field: Incyte: Research Funding; Prolong Pharmaceuticals: Research Funding; Astellas: Research Funding; NKT Therapeutics: Honoraria, Research Funding. Shows: PCORI: Research Funding. Saheed: PCORI: Research Funding. Varadhan: PCORI: Research Funding. Segal: PCORI: Research Funding. Wang: PCORI: Research Funding. Brooks: PCORI: Research Funding. Frymark: PCORI: Research Funding. Griffin: PCORI: Research Funding. Kincaid: PCORI: Research Funding. Burgess: PCORI: Research Funding. Robertson: PCORI: Research Funding. Proudford: PCORI: Research Funding. Green: PCORI: Research Funding. Piehet: PCORI: Research Funding. Wang: PCORI: Research Funding. Huang: PCORI: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal